Neutropenia is a medical condition identified by an unusually low level of neutrophils, a type of white blood cell essential for combating infections. Neutrophils play a critical role in the immune system by targeting and destroying harmful bacteria and fungi. A deficiency in these cells increases the risk of infections, making it vital to understand the symptoms, causes, and treatment options associated with neutropenia.
In this article, we’ll explore Neutropenia, its symptoms, causes, and available treatment options, providing a thorough understanding of this disorder and the ways for it to be managed effectively.
Symptoms of Neutropenia
Neutropenia itself does not directly cause symptoms. Instead, the complications arise from infections due to the weakened immune defence. Common symptoms include:
Infections
Patients with neutropenia are particularly vulnerable to recurrent infections due to the reduced number of neutrophils, which are necessary for fighting off harmful bacteria. Common areas affected include the respiratory tract, sinuses, and skin. As the immune system struggles to respond adequately, infections often become more severe and frequent. Respiratory infections like pneumonia or sinusitis are especially concerning, as they can lead to complications without proper treatment.
Fever
Fever is one of the most common signs of infection and may point to an underlying issue, such as neutropenia. Since neutrophils are responsible for fighting off infections, their deficiency makes the body less effective at controlling bacterial or fungal invaders, resulting in higher body temperatures.
Mouth Ulcers
Another common sign of neutropenia is mouth ulcers, which are painful sores in the mouth. Eating and drinking can be uncomfortable due to these sores, which usually appear on the inner cheeks, tongue, or gums. Neutropenia weakens the immune system, making it more difficult to fight off bacterial or fungal infections that may cause ulcers. These sores have the potential to get infected, which could exacerbate an already compromised immune system and cause more issues.
Swollen Gums
Swollen gums are a frequent symptom in individuals with neutropenia, often resulting from bacterial overgrowth due to the body’s diminished ability to control microbial populations. Gums may become red, inflamed, and sensitive, and patients may experience bleeding or discomfort while eating or brushing their teeth.
Fatigue
Persistent tiredness or fatigue is a common issue for individuals with neutropenia, as the body is constantly fighting infections. The immune system is overstressed, requiring more energy to deal with bacterial, viral, or fungal pathogens. Also, the constant presence of infections can cause the body to become drained, leading to a feeling of fatigue that can interfere with daily activities and overall quality of life.
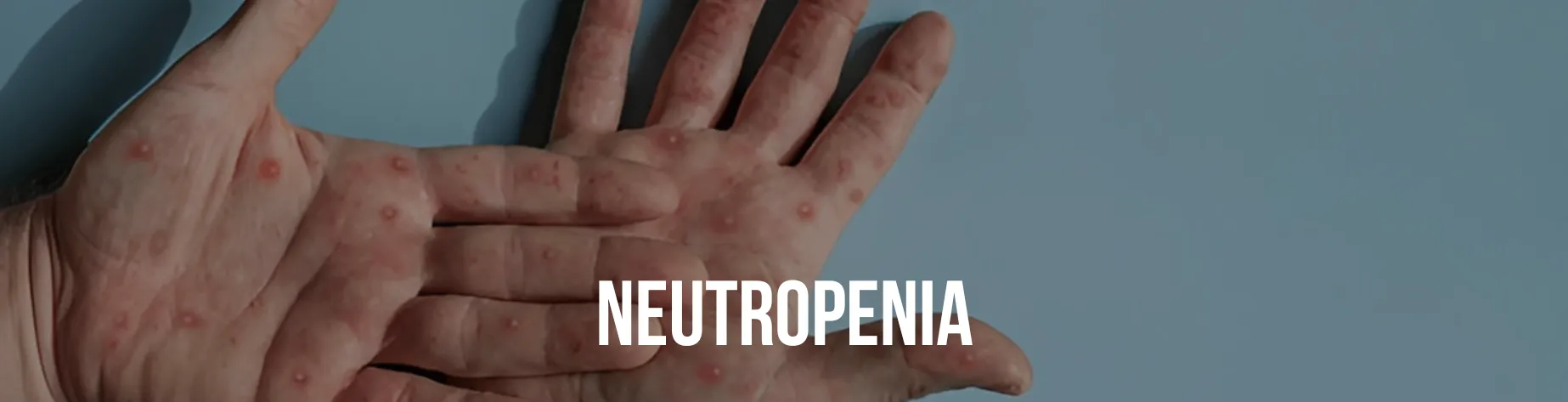
Skin Lesions
Unusual or persistent skin lesions, such as rashes, boils, or abscesses, are often seen in neutropenic patients due to the body’s inability to defend against skin infections. These lesions may be painful, swollen, or infected and can sometimes be a sign that bacteria have entered through cuts or weakened skin areas. Because neutropenia reduces the body’s ability to heal and fight off infections, these skin issues may last longer and require medical intervention.
Delayed Healing
Injuries, wounds, or cuts that take longer to heal are among the symptoms of neutropenia. It is due to the fact that the body’s ability to heal damaged tissue and prevent infections that could hinder the healing process is directly impacted by the immune system’s decreased production of neutrophils. Even minor injuries may take longer to heal, and if not properly cared for, they can lead to more serious infections that complicate recovery.
Causes of Neutropenia
Neutropenia can arise from a variety of underlying conditions, treatments, or external factors. It is classified into congenital (present at birth) or acquired (developed later). The key causes include:
Bone Marrow Disorders
One of the leading causes of neutropenia is bone marrow disorders, which affect the body’s ability to produce neutrophils. Aplastic anaemia, for instance, is a condition in which the patient’s bone marrow fails to produce enough blood cells, including neutrophils. Leukaemia, a type of cancer that affects bone marrow and blood, can also reduce neutrophil production due to abnormal white blood cell growth. Myelodysplastic syndromes, a group of disorders caused by malformed or dysfunctional blood cells, can impair bone marrow function, leading to neutropenia.
Autoimmune Conditions
Autoimmune diseases can contribute to neutropenia, which occurs when the immune system unknowingly attacks the body’s neutrophils. Other autoimmune disorders, like systemic lupus erythematosus (SLE) and rheumatoid arthritis, can also lead to neutropenia as a result of the immune system’s inflammatory responses. In these cases, neutrophil depletion may occur as part of the broader autoimmune activity that affects various tissues and organs in the body.
Infections
Certain infections can disrupt neutrophil production or cause their destruction, leading to neutropenia. Viral infections like HIV, hepatitis, and Epstein-Barr virus are known to impact bone marrow function, either by directly affecting the marrow or by triggering immune responses that reduce neutrophil levels. Also, severe bacterial infections can sometimes overwhelm the body’s immune system, depleting neutrophil stores or suppressing their production.
Medications
Another significant cause of neutropenia is medications, especially those that interfere with bone marrow function. Chemotherapy drugs used to treat cancer, often suppress the bone marrow, leading to a decreased production of neutrophils. Certain antibiotics, anticonvulsants, and antipsychotics are also linked to neutropenia as a side effect, either by directly affecting the bone marrow or through an immune-mediated response.
Nutritional Deficiencies
Essential vitamin and mineral deficiencies can also contribute to neutropenia. A lack of folate, vitamin B12, or copper can impair bone marrow production, reducing the neutrophil count. These nutrients are vital for proper blood cell development, and their absence can lead to various haematological disorders, including neutropenia.
Treatment of Neutropenia
Treatment for neutropenia depends on its severity, duration, and underlying cause. Key approaches include:
Addressing the Underlying Cause
The first step in treating neutropenia is often to address the underlying cause of the disorder. If an infection causes neutropenia, appropriate antibiotics or antifungals are prescribed to treat the infection and prevent further complications. In cases where medications are responsible for neutropenia, the doctor may decide to either discontinue the medication or replace it with one that does not affect neutrophil production.
Medications
Specific medications can stimulate the production of neutrophils or reduce immune system activity in cases of autoimmune neutropenia. Granulocyte Colony-Stimulating Factor (G-CSF) is a key medication used to stimulate the bone marrow to produce more neutrophils. It is particularly effective in neutropenia caused by chemotherapy or certain blood disorders.
Corticosteroids are often prescribed for autoimmune-related neutropenia. They suppress the immune system’s attack on neutrophils, helping to preserve their levels in the bloodstream. In some cases, immunoglobulins are used to boost the immune system in individuals with autoimmune or congenital neutropenia, helping to reduce infections and support the body’s natural defences.
Nutritional Support
For neutropenia caused by nutritional deficiencies, supplementing with vitamin B12, folate, or copper can be crucial in restoring normal neutrophil production. These nutrients play a significant role in the development of blood cells, and a deficiency can lead to reduced neutrophil levels. Regular monitoring of vitamin and mineral levels, along with dietary adjustments or supplementation, can help prevent or treat neutropenia caused by poor nutrition.
Preventive Measures
Patients with neutropenia need to take preventive measures to reduce the risk of infection, as their immune systems are compromised. To prevent the spread of bacteria and viruses, it is vital to wash hands regularly and maintain good personal hygiene. During flu seasons, neutropenic individuals should avoid crowded places to minimise exposure to infectious agents. Also, prophylactic antibiotics may be prescribed for patients undergoing chemotherapy or those with prolonged neutropenia to prevent bacterial infections before they occur.
Conclusion
In conclusion, neutropenia is a complex condition that demands timely recognition and management to mitigate the risk of infections. Understanding its symptoms, identifying the root cause, and implementing targeted treatments can significantly improve outcomes for affected individuals. Advances in medical care, including G-CSF therapies and bone marrow transplants, have transformed the prognosis for many patients with neutropenia, enabling them to lead healthier, more secure lives.